Background: Sickle cell disease (SCD) consists of a group of hemoglobinopathies inherited in an autosomal recessive pattern whereby a single point mutation results in the formation of a hemoglobin protein with altered structure. Many of the complications of SCD and their end organ manifestations are the result of a vaso-occlusive process. These include acute chest syndrome, dactylitis, myocardial infarction, stroke, venous thromboemboli, avascular necrosis, and acute vaso-occlusive episodes (VOEs). VOEs are the most common reason for a patient with SCD to seek medical attention. This care is often provided at an emergency department (ED). It has been well documented that the management of VOEs are often delayed and fail to follow published guidelines. Numerous efforts have been undertaken to ensure appropriate and timely analgesic administration to patients with SCD who are experiencing a VOE. One such intervention is the creation of an infusion center (IC) that has the capability to administer parenteral opioids while avoiding the delays associated with an ED visit.
Objectives: This study aims to evaluate the impact of a dedicated IC that was established for the treatment of SCD VOEs. The goal of the IC is to provide timely and appropriate pain management in an effort to reduce ED visits and hospital admissions related to treatment of VOEs in patients with SCD. The IC was available to adult patients with SCD who regularly sought care at our hospital and who did not have a care plan that excluded the administration of parenteral opioids.
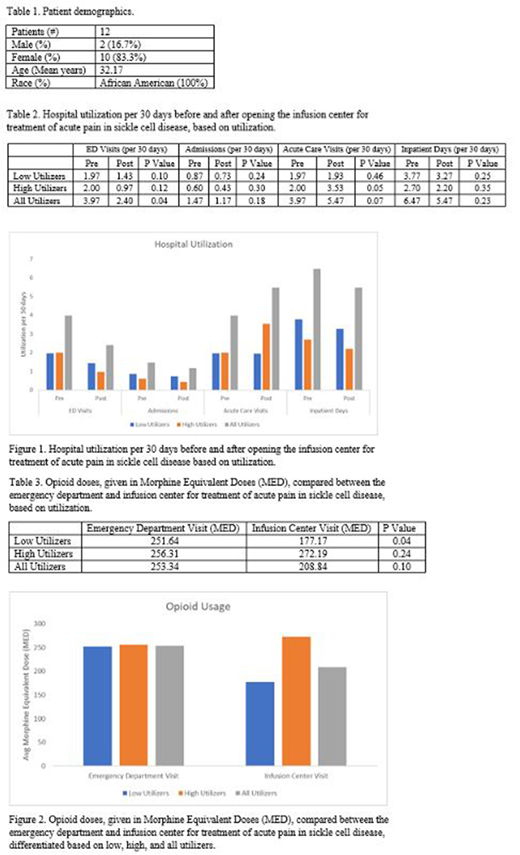
Methods: This is an observational, retrospective study comparing the rates of hospital utilization before and after the opening of a dedicated IC for patients treated for SCD VOE at a single, urban medical center that regularly provides care for approximately 150 adult patients with SCD. We compared the rates of ED visits, hospital admissions, and length of stay for six months prior and four months following the opening of the IC. Hospital utilization was standardized before and after the intervention using 30-day rates. Additionally, opioid usage, measured in Morphine Equivalent Dose (MED) was compared between the ED and the IC.
Results: A total of 12 patients (Table 1) utilized the IC during the 4 months after its opening (6/20/19 - 10/16/19). During this time there were 92 total visits to the IC. Four patients were noted to be high utilizers accounting for 77 (83.7%) of the 92 visits (median = 20 visits, range 12 - 25). The other 8 patients were low utilizers and accounted for 15 (16.3%) of the visits (median = 2, range 1 - 4). Following implementation of the IC, there was found to be a statistically significant decrease in ED visits (pre- = 3.97/30d vs post- = 2.40/30d; p = 0.04) (Table 2, Fig. 1). No significant difference was found in hospital admissions (pre- = 1.47/30d vs post- = 1.17/30d; p = 0.18) or inpatient days (pre- = 6.47/30d vs post- = 5.47/30d; p = 0.23). The total number of acute care visits (sum of ED and IC visits) was found to increase after the opening of the IC, although the change was not statistically significant (pre- = 3.97/30d vs post- = 5.47/30d; p = 0.07). The change in acute care visits was largely driven by an increase in visits from the high utilizers (pre- = 2.00/30d vs post- = 3.53/30d; p = 0.05). In terms of parenteral opioid administration, there was a statistically significant decrease in amount of opioids given in the IC compared to the ED (ED = 251.64 MED vs IC = 177.17 MED; p = 0.04), although this was only seen in the low utilizer group (Table 3, Fig. 2). There was no significant difference in opioid doses received for the high utilizers (ED = 256.31 MED vs IC = 272.12 MED; p = 0.24) and for the group as a whole (ED = 253.34 MED vs IC = 208.84 MED; p = 0.10).
Conclusion: The introduction of an IC for the management of SCD VOE led to a significant decrease ED visits but also led to an increase in overall acute care visits, although this was not statistically significant. This increase was largely driven by a subset of this population considered high utilizers. Additionally, the use of the IC was not associated with a decrease in the total amount of parenteral opioids that were administered. However, for the low utilizer group there was a decrease in parenteral opioid administration. The IC did not reduce admissions and duration of hospitalization in this population. Overall, the IC had variable success and further refinement of how it is used should be undertaken to ensure quality care for patients with SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal